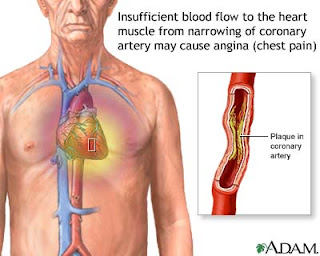
- Due to myocardial ischaemia, presents with chest pain or tightness that is relieved by rest
- May radiate to jaw or arm
- Other precipitants – emotion, cold weather and heavy metals
- Associated symptoms – dyspnoea, nausea, sweatiness, faintness
Causes
- Most commonly atheroma
- Rarely – anaemia, AS, tacharrhythmias, HOCM and arteritis/small vessel disease
Types
- Stable angina – induced by effort relieved by rest
- Unstable angina – angina of increasing frequency or severity (associated with increased risk of MI)
- Decubitus angina – precipitated by lying flat
- Prinzmental’s angina – caused by coronary artery spasm
Tests
- ECG – may show ST depression and T wave inversion or flattening from previous MI
- Exercise ECG
- Thallium test
- Coronary angiography
- Exclude precipitating factors – anaemia, diabetes, hyperlipidaemia, thyrotoxicosis, GCA
Management
- Change lifestyle
- Treat modifiable risk factors – hypertension, DM
- Aspirin – 75-150mg/24hr, reduces mortality by 34%
- ?-Blockers – Atenolol 50-100mg/24hr, unless CI (asthma, COPD, LVF, bradycardia, coronary artery spasm)
- Nitrates – for symptoms give GTN spray or sublingual tabs every 30mins. For prophylaxis take regular oral nitrate e.g. isosorbide mononitrate 10-30mg BD or slow release nitrate 60mg/24hr
- Calcium channel antagonists – amlodipine or diltiazem
- If total cholesterol is >4mmol/L give a statin
- Consider adding a K+ channel activator
Percutaneous transluminal coronary angioplasty (PTCA)
- Involves balloon dilation of the stenotic vessel
- Indications – poor response or tolerance to medication, refractory angina in patients not suitable for CABG, previous CABG, post-thrombolysis in patients with severe stenosis or positive stress test
- Comparison wit PTCA and drug along show that PTCA may control symptoms better but with increased risk of early cardiac event
- Complications – restenosis (20-30% in 6mths), emergency CABG (<3%), MI (<2%), death (<0.5%)
- Stenting reduces rates of restenosis and need for bail out CABG
- Drug coated stents and antiplatelet drugs reduced rates of restenosis
CABG
- Indications – left main stem disease, multiple vessel disease, distal vessel disease, patient unsuitable for angioplasty, failed angioplasty
- Comparisons between CABG and PTCA showed that CABG was better for symptom control and had a lower reintervention rate but required a longer recovery and inpatient stay
EmoticonEmoticon