Cardiology: Anaphylactic Shock
Allergic reactions can vary greatly in their severity. This may depend on the quantity and route of allergen exposure, and on the individual. The most severe reactions can result in death, and sometimes cardiac death might occur without respiratory symptoms.
Severe allergic reactions are those producing severe symptoms which are not immediately life-threatening such as generalised urticaria, mild bronchospasm or angioedema.
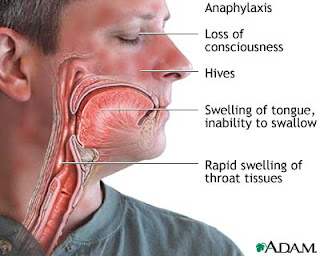
Anaphylaxis is the term used for acute allergic reactions producing life-threatening features:
o Hypotension and shock,
o Severe bronchopasm which might cause wheeze and stridor
o Laryngeal oedema.
- Other features of an allergic reaction may be present including angioedema, puritis, urticaria, tachycardia, nausea and vomiting. These are features that typically affect the airways, skin and GI tract.
- Not all patients will suffer from all symptoms, and only one area may be affected. However, this reaction is typically the same for an individual patient upon each exposure to the antigen.
- Typical signs are similar to those of shock and might include:
- ↑Resp Rate (e.g. >30)
- ↑Pulse (e.g. >120)
- ↓BP
- There are no investigations, and the diagnosis is clinical – there is no time for investigations
- A history of atopy
- Does NOT increase the risk of anaphylaxis
- DOES increase the risk of death when anaphylaxis occurrs
Common causes include: foods (e.g. nuts, seafood); drugs (e.g. antibiotics, NSAIDs), venom (e.g. bee, wasp) and latex.
- Peanut and latex allergies may be airborne!
There is an increased risk of anaphylaxis in those with a family history of atopy, bronchial asthma and those on corticosteroid/ACEi/beta-blocker therapy.
Mechanism: exposure of susceptible individuals to allergen results in the production of IgE antibodies and the release of inflammatory mediators from mast cells. Local histamine release causes bronchoconstriction, vasodilation and increased vessel permeability.
- Anaphylaxis requires a prior exposure to the antigen. I.e. there is a sensitisation reaction that occurs on first exposure (which does not result in anaphylaxis), and it is only on a second exposure to an allergen, that anaphylaxis may occur.
- Anaphlyactoid reactions are clinically indistinguishable from anaphylaxis, however, they are not IgE mediated, and do not require a prior exposure. They occur via direct stimulation of mast cells, and can be caused by agents such as NSAIDs, opioids, blood transfusions and even exercise.
Management:
- Initial ABC approach – secure airway and obtain IV access. Give 100% oxygen. Lower head of bed to restore blood volume. Consider intubation
- Remove the cause if possible.
- Adrenaline 0.5mg IM, repeated every 5min as required (monitor BP, pulse and respiratory function, keep giving until BP recovered).
- Patients who do not respond to epinephrine should be quickly intubated – which reduces the risk of cricothyroidotomy.
- Beware the dose of adrenaline – the IV dose is much lower than the IM dose!
- Antihistamine (e.g. 10mg chlorphenamine) and corticosteroid (e.g. 200mg hydrocortisone) IV.
- Monitor BP and give IV saline as appropriate.
- Treat asthmatic wheeze – typically inhaled β2-agonists
Long-term management: Identify allergen and educate patient about self-injected adrenaline.
Notes by Nicole McGrath and Tom Leach